Everything You Need to Know to Heal Your Scars
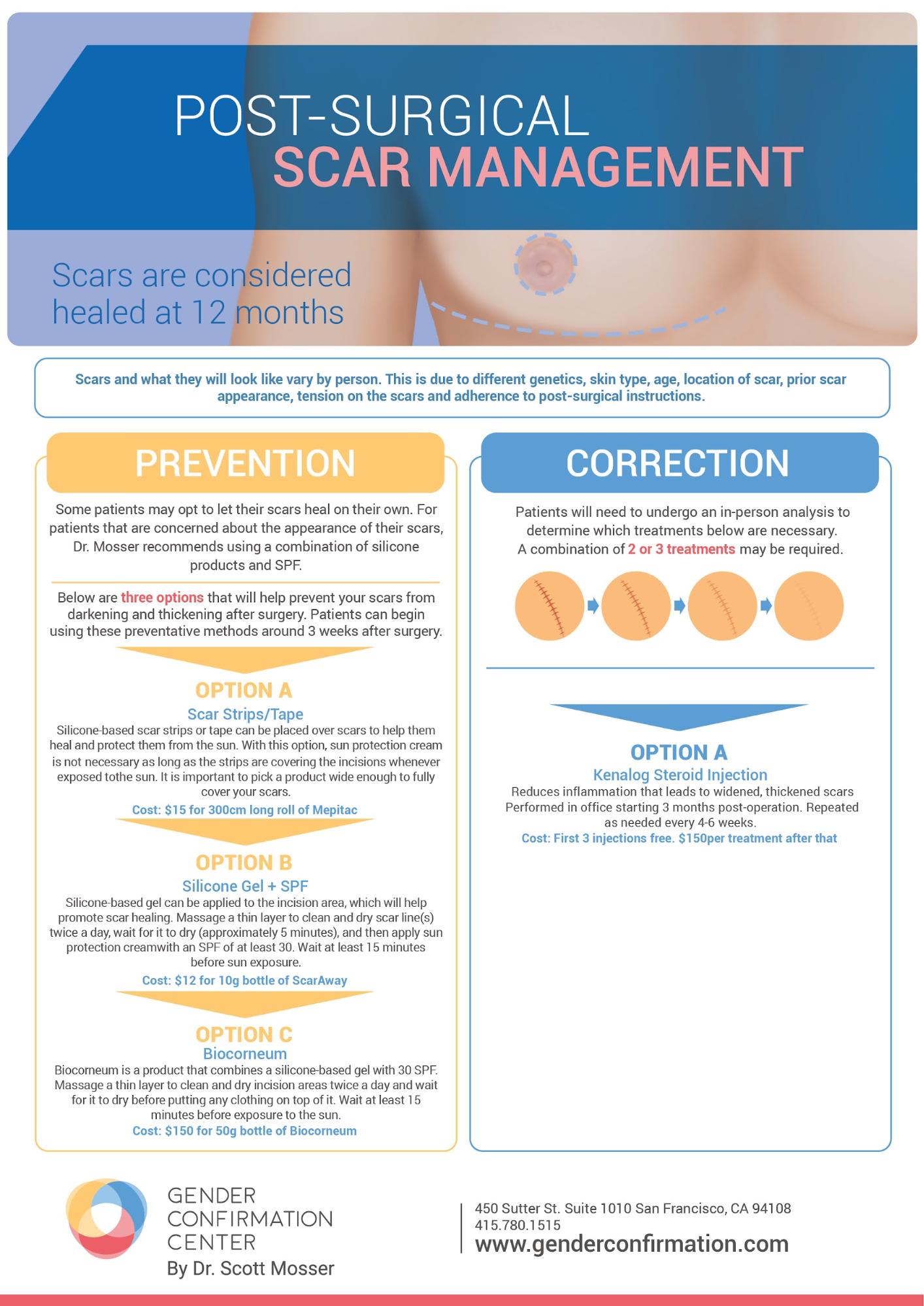
Since many gender affirming surgeries–including top surgery, breast augmentation, facial surgery and many bottom surgeries–involve making incisions on the skin to change the body’s form, a part of the long-term recovery process for surgery involves taking care of scars. In this article we address common patient concerns around scarring by going over our board-certified surgeons’ recommendations for preventing and treating scar discoloration and thickness. We also touch on hypertrophic and keloid scars as well as scarring for patients with richer or darker skin tones. If you would like a more concise breakdown of our prevention and treatment recommendations, you can find them in this downloadable PDF, pictured below.
Incisions to Scars: When to Begin Treatment?
A surgical incision becomes a scar once it closes up. Surgical incisions, unlike normal cuts, are skillfully made to maximize a patient’s healing process. Still, we recommend that patients carefully follow incision and scar care instructions during the first year after surgery to reduce discoloration, thickness and prevent chronic pain. This is because scars are not considered fully healed until 12 months have passed since the incision was made. For example, we recommend that patients keep their incisions and scars out of direct sunlight, or to at least use a sunscreen with an SPF of at least 50, to protect them from UV exposure, and therefore further discoloration during the entire first 12 months after surgery.
For the first three weeks after surgery, what you will be asked to do to care for your incisions will depend on the type of surgery you underwent. Most patients will have surgical dressings on until their first postoperative appointment with their surgeon, about a week after surgery. After the postoperative appointment, patients may have gauze and bandages that they are instructed to replace during this time. Again, your surgical team will give you individualized instructions based on the specific surgery you undergo and will provide you with supplies if necessary.
At about 3 weeks post-op your incisions should be closed up, meaning that scar care can begin. Once your surgeon has given approval around the three week mark, you can begin to treat the scars with silicone gel and/or silicone scar tape if you are interested in reducing the visibility of your scars long-term. It is of the utmost importance that patients also begin scar massage: applying pressure to them in a circular motion with their fingers to break up scar tissue forming beneath the skin. We recommend that patients give themselves scar massages, applying silicone gel into the tissue, twice a day at least for the first three months after surgery. Scar massages should continue throughout the first year of recovery to help break up fibrosis and prevent any chronic pain, such as post top surgery pain syndrome.
Generally, scars will continue to get more pigmented and raised for the first 3 months after surgery, before they begin to soften and lose their pigmentation. Scars will continue to heal over the course of the first 12-18 months after surgery, and a combination of scar massage, applying silicone ointment, and keeping scars out of the sun can all help promote scar healing.
Prevention & Treatment Tips
Prior to surgery, there are many steps a patient can take to prevent scar discoloration and reduce their texture…
- If you currently smoke, avoiding tobacco use for at least 3-6 weeks before and after surgery is one of the easiest ways to improve your body’s healing response.
- Eating a nutritious diet that contains adequate protein, zinc and vitamin C, all of which have been clinically proven to accelerate healing, is another step you can take in advance of your procedure.
- Following surgery, it is important to keep your scars out of the sun (or wear strong sunscreen) for at least one year. Over-the-counter topical treatments like Scarguard and Bio-Oil have been shown to speed up wound healing and improve the appearance of scars.
- Using silicone scar cream, silicone sheeting or compression tape is also an effective way to treat scars because they create an atmosphere of moisture, which prevents the build-up of collagen that can cause scarring. Your surgeon can recommend specific scar treatment for you based on your skin type.
If topical treatments are not helpful, there are several other treatments that can improve the appearance of scars once fully healed, such as:
- Steroid injections
- Surgical revision
- Laser scar removal
- Microdermabrasion
- Medical needling
Hypertrophic and Keloid Scarring
Regardless of perfect suturing of your incisions by your surgeons, some patients can develop either hypertrophic or keloid scars–of which the latter is often genetically predetermined. Hypertrophic scars are what we call scars that develop a thick, ropy texture as a result of tissue build up or fibrosis. More rarely, patients can develop keloid scars, which are scars that thicken and grow into the surrounding healthy tissue.
Hypertrophic and keloid scars can be treated with scar massage, silicone scar therapy (applying silicone scar cream or scar tape), microneedling therapy and the three scar therapies mentioned in the PDF pictured above. If a patient is not satisfied with or interested in these options to help flatten scars and reduce discoloration, they can request a revision surgery to excise the original scars and create new ones.
Scarring for Patients with Darker Skin Tones
For patients of color with a richer skin complexion, there is risk of hypopigmentation. Hypopigmentation involves the lightening of scar tissue, making scars more visible compared to the surrounding, darker skin tone. Following the guidelines mentioned above can help reduce the risk of hypopigmentation. Likewise, if scar therapies are not enough to reduce hypopigmentation to your desired degree, you can also pursue medical tattooing services to camouflage your scars with the surrounding pigment using ink. Regardless, if this is a concern of yours, we encourage you to speak with your surgeon about options for scar placement and hypopigmentation treatment for patients with higher levels of melanin in their skin.
Identifying & Treating Keloid & Hypertrophic Scars
In this informational video, Dr. Alexander Facque (he/him) explains the difference between keloid and hypertrophic scars as well as how they can be treated.
Request a Free Surgical Consultation Today.
All virtual and in-person consultations with our board-certified surgeons are free. Once you fill out this form, our patient care team will reach out and guide you through every step to get to surgery.