Understanding Vaginoplasty Surgery
Medically reviewed by Jennifer Richman on June 13, 2025.
What is Vaginoplasty?
Vaginoplasty is a form of gender-affirming bottom surgery or sex reassignment surgery that creates a vaginal canal alongside a vulva or external genitalia, such as a clitoris with full sensation, labia majora, and a shortened urethra.
This procedure is a good match for individuals looking to have a vulva with a clitoris, erogenous sensation, and a vaginal canal of approximately 5-6” in depth that can be used for penetrative solo or partnered sex. To maintain depth and width of the vaginal canal, lifelong dilation is required.
Several peer-reviewed studies have demonstrated that qualified candidates who undergo vaginoplasty with experienced, board-certified providers have extremely high rates of general satisfaction and satisfaction with sexual function.
All of the Gender Confirmation Center (GCC)’s bottom surgery procedures are performed by Dr. Ellie Zara Ley (she/her/they). She is a board-certified plastic surgeon and the only transgender woman of color to offer a full-spectrum specialization in gender-affirming top surgery, bottom surgery, facial surgery, and body contouring.
Dr. Ley is a leader in the field of genital reconstruction surgeries, using only tried-and-true methods backed by longitudinal research for her patients. You can request a free in-person bottom surgery consultation with her for a first-time or revision procedure here.
Surgical Options: The Different Types of Vaginoplasty
Penile-Inversion Vaginoplasty
The creation of a vaginal canal can involve a variety of techniques. The most common vaginoplasty procedure is the penile-inversion vaginoplasty. After the removal of the penis, called a penectomy, some tissue is retained as the urethra is shortened, erectile tissue is buried into the pelvic region to create a clitoris, and the skin of the penis is turned inside out to create the lining of the vagina. The testes and scrotum are removed, in procedures called orchiectomy and scrotectomy, and the scrotal skin is also used to create the lining of the vaginal canal. Patients who are short on penile and scrotal skin may need 1 or 2 grafts from the hip region in order to line the vaginal canal. Please note that this is the only method that Dr. Ley performs.
The penile inversion method is preferred by patients because of its durability for penetration, and it is the only technique that has longitudinal evidence to back its effectiveness.
Peritoneal Pull-Through and Robotic Vaginoplasty
Patients can also have their vaginal canal lined with the mucus membrane of the rectal tissue or the internal abdominal wall. The advantage of this method is that it may allow for the possibility of self-lubrication, although results have been shown to be inconsistent.
Some surgeons perform vaginoplasties using a robotic method. The robotic technique, also called the robotic peritoneal vaginoplasty, involves the creation of incisions around the navel where robotic surgical instruments are inserted into the abdomen. Visualization of the placement of the vaginal canal is achieved through a high definition camera and the surgeon constructs the canal from the inside using the peritoneum (lining of the abdominal wall). The advantage of this method is that it can allow for less skin grafts to be taken to create a longer vaginal canal.
Please note that Dr. Ley only offers the penile-inversion technique at this time, as it has the most long-term evidence to back its effectiveness.
The Two-Staged Approach to Vaginoplasty: Improving the Vulva’s Appearance
At the GCC, Dr. Ley offers an innovative two-stage approach to traditional vaginoplasty. The first stage of a traditional vaginoplasty creates the vaginal canal, clitoris and labia majora. About 5 months later, if the vagina and vulva have healed properly, a clitoral hood and labia minora are constructed.
By splitting up this operation into two stages, the vulva has a better chance of healing properly. This has given Dr. Ley’s patients more consistent results, leaving them more satisfied with the outcome of their surgery and less likely to request a revision procedure later on.
“Zero-depth” Vaginoplasty or Vulvaplasty
A vulvaplasty is very similar to a vaginoplasty in all aspects, except a vaginal canal is not created. A vulvaplasty includes the creation of a vulva, clitoris and labia majora using tissue from the penis, scrotum, and surrounding tissue. This procedure is selected by patients who would like a vulva, but are have no interest in having penetrative sex through a vagina nor do they have an interest in having to dilate their vaginal canal to maintain it. Most patients can still experience orgasm and full erotic sensation through their clitoris as early as 3 months post-op.
The majority of patients who undergo a vulvaplasty are happy with their choice and do not desire to have a vaginal canal. However, if someone does decide later on that they would like a vaginal canal after vulvaplasty, this is possible.
What is a penile-preserving vaginoplasty?
Penile-preserving vaginoplasty is exactly what it sounds like: a vaginal canal is created without removing the penis. In this case, the vaginal canal is crafted not using penile tissue, but using scrotal tissue and grafts that come from the hips. Lifelong dilation is required after this procedure.
Preoperative and Candidacy Requirements
To qualify for vaginoplasty, patients must meet the following criteria:
- Age 18 or older
- A support letter from a licensed gender health professional who has a well-documented and established provider-patient relationship over an extended period of at least nine months. The letter should include the following elements:
- A gender dysphoria diagnosis
- Any other existing psychiatric diagnoses and whether or not they impact the patient’s readiness for surgery
- A statement that informed consent has been obtained from the patient: that they understand the risks, benefits, and potential long-term effects (e.g., permanent infertility) of bottom surgery.
- Continuous hormone therapy for a minimum of 12 months (while not required by the GCC, many insurance companies include this as a part of their clinical guidelines)
- Vaginoplasty patients should undergo hair removal in the months leading up to surgery.
- Nonsmokers or individuals who quit tobacco and nicotine consumption at least 6 weeks prior to surgery
- Good overall physical health
- Vaginoplasty patients must have a BMI of 34 or less, while vulvaplasty patients must have a BMI no greater than 38
- Reliable support system including friends or family, mental health professionals as needed, and a safe home environment
- Commitment to adhering to post-operative care (e.g., dilation protocols)
Do I need to stop taking estrogen for surgery?
Many providers ask patients to stop estrogen hormone replacement therapy (HRT) 1-2 weeks prior to surgery to reduce the risk of blood clots. Patients who have personal or health concerns about suspending estrogen therapy can speak with our surgical team about the possibility of waiving this requirement for their specific case.
Frequently Asked Questions about Vaginoplasty
Do I need to undergo laser hair removal or electrolysis to get an MTF vaginoplasty?
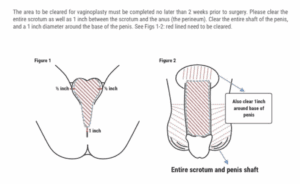
To undergo a penile-inversion vaginoplasty, patients should undergo permanent hair removal prior to their procedure. Laser hair removal and/or electrolysis of the penis shaft and scrotum are essential to prevent complications from hair growth inside of the vaginal canal and/or in the vulva. Specifically, these complications include infection, collections of hair, and dyspareunia (pain during sexual intercourse).
Will a transgender vagina look like a cisgender vagina?
All vaginas and vulvas are unique in their appearance. While there are certain anatomical differences between natal vaginas and vaginoplasty results––such as the thickness of the urethral tube––Dr. Ley’s two-stage technique was specifically designed so that the vulva of her patients resembles natal vulva anatomy. By performing a labiaplasty 5 months after the vaginoplasty, the vulva has a better chance of healing properly, and the surgeon has greater control over the details of the appearance of the labia, clitoral hood, urethra, and clitoris.
Can a minor or adolescent undergo a vaginoplasty?
No, a patient must be at least 18 years of age and provide proper documentation to be eligible for a vaginoplasty or other bottom surgery procedures. Documentation must demonstrate the patient’s ability to comprehend the irreversible nature of the procedure, their mental fitness to participate in the informed consent process, and that they meet the gender dysphoria diagnostic criteria.
Is a vaginoplasty painful?
A vaginoplasty occurs under general anesthesia, meaning the patient will be unconscious and unable to feel anything during the procedure. Patients will be prescribed pain medications after surgery to manage pain.
Can I orgasm after a vaginoplasty?
Yes. The clitoris is made by burying the glans of the penis, so it maintains a heightened, erotic sensitivity since the original nerve and blood supply is preserved. Patients typically regain full sensation and may experience orgasm 3-9 months after the clitoris is constructed.
How much does a vaginoplasty cost? How much does MTF bottom surgery cost?
For patients without insurance, a vaginoplasty can cost $23,000 – $24,500. A vulvaplasty’s out-of-pocket cost can range from $20,500 – $22,000, and a labiaplasty’s cost can range from $8,500 – $16,000. Please note that the following ranges are estimates. These can vary by provider and the details of an individual’s unique surgical plan. Additionally, these estimates do not include facility fees, hospital fees, anesthesiology fees, or pathology fees.
Will my insurance cover a vaginoplasty?
Many insurance providers recognize gender-affirming bottom surgery as a medically necessary form of treatment for gender dysphoria. With the proper requirements fulfilled, such as one or two support letters from a licensed mental health professional or other gender care provider, insurance can cover part or all of the costs of the procedure. For more information on insurance coverage, click here.
Benefits, Risks & Complications
Most patients who undergo surgery with an experienced, board-certified surgeon can expect to experience minimal risks. Most surgical complications that arise can be resolved without the need for the patient to undergo a later revision surgery. Patients can reduce their risk of complications by taking the following steps:
- Stop all smoking at least 3 weeks before and after surgery
- Do not consume alcohol at least 1 week before and one week after surgery
- Keeping any chronic health conditions well-managed
Complications
These complications can usually be treated without the need for an additional revision surgery. Complications can include:
- Wound openings
- Hematomas
- Vaginal granulation
- Abnormal urinary stream
- Blood in the urine
- Urinary fistulae (holes in the urinary tract)
- Urinary tract infections
Serious Risks
Serious risks can include:
- Excessive bleeding
- Blood clots
- Infections
- Severe pain levels that are unresponsive to medications
- Fever
- Abnormal swelling in the groin or lower leg
- An inability to keep foods/liquids down
- Shortness of breath, pain in your chest, lightheadedness, or dizziness
Notify your provider immediately of any concerning symptoms, whether listed above or not. You may need to go to an emergency room immediately. For more information, click here.
Gender-Affirming Vaginoplasty Recovery
Initial Healing
Vaginoplasty and Vulvaplasty patients can expect to stay in the hospital for at least 3 nights after surgery to monitor their recovery closely. The recovery process generally takes 6-8 weeks, although consistent dilation of the vaginal canal is essential during the first six months to a year. For more detailed instructions, click here.
Bleeding and spotting are expected from the incisions for up to 6 weeks post-op. It is normal to experience vaginal discharge in the first few months post-op. Swelling and bruising should also greatly subside by this time. That said, patients will likely not get a sense of the final appearance of their vulva until 3-6 months post-op.
Dilation
Lifelong dilation is required when a vaginal canal is created for a primary vaginoplasty or a vaginal deepening/widening revision surgery. You will receive guidance and support from your surgical care team as you begin dilating after surgery.
Catheter
After a vaginoplasty, a patient can expect to have a urinary catheter for about 8 days post-op.
Sexual Activity
We require patients to wait 3 months to have penetrative sex. Patients commonly feel a return of erotic sensation to the clitoris 3-9 months after surgery and regain the ability to orgasm at this time.
It is normal to take some time to learn and rediscover your new body. Starting gently and slowly is a good approach, with open verbal communication with your partner, if one is present.
Request a Free Surgical Consultation Today.
All virtual and in-person consultations with our board-certified surgeons are free. Once you fill out this form, our patient care team will reach out and guide you through every step to get to surgery.