Emotional Recovery From Surgery: Depression Symptoms, Coping, and Support
Written by Giovanna D’Ambrosio. Medically reviewed by Dr. Scott Mosser on April 28th, 2025.
Recovering from surgery can be a physically and emotionally challenging process. Many people experience postoperative depression, even when their procedure is successful and free of complications. Feeling emotional after surgery is a common part of the healing process. This can arise from factors such as stress about regaining full strength, experiencing pain and inflammation, the impact of medications on mood, the body’s reaction to anesthesia, and limited mobility during recovery.
Post-surgery depression and anxiety may manifest in different ways—persistent sadness, exhaustion, and a loss of interest in activities you used to enjoy. Some refer to this emotional phase as the post-surgery blues or post-operative depression, a temporary but distressing part of healing.
Postoperative depression and anxiety can occur after any procedure, but it is especially important to discuss after gender-affirming surgery, as patients often expect only feelings of happiness and celebration about what is to come. Recognizing that emotional ups and downs are a common part of the healing journey can help ease the recovery process. Practicing patience, self-care, and seeking support from loved ones or healthcare professionals can make a significant difference in navigating post-op depression and anxiety with resilience.
Causes: Why Might I Feel Depressed After Surgery?
Experiencing postoperative depression is a significant event, both physically and emotionally. Our bodies often perceive surgery as a trauma, leading to natural physiological and psychological responses during recovery. As your body focuses on healing, you may feel a temporary dip in energy or mood, such as sadness or low motivation. This is your body’s way of signaling the need to rest and recuperate.
While many anticipate a surge of positive emotions after gender-affirming surgery, the reality is that it is common to also feel negative emotions at first due to the difficulties of recovery. . Your body is adjusting, emotions are shifting, and the change in routine can bring unexpected feelings. Acknowledging these emotions is an important part of the healing process. Practicing patience and compassion can help you navigate this transition.
Several factors can contribute to postoperative depression:
- Psychiatric predispositions: Receiving a diagnosis of depressive disorder before surgery, or having a history of untreated depression or anxiety, may pose a significant risk factor.
- Emotional risk factors: Stressors may include missing work, managing financial strain, and depending on others for support, especially when needs are not fully met. If the surgery is associated with a serious health condition, concerns about mortality and overall well-being can present additional emotional challenges.
- Anxiety: When worries about outcomes, recovery, or complications become overwhelming, they can heighten the risk of post-op depression. Anxiety also becomes a concern when it renders stress unmanageable or hinders realistic expectations for healing.
- Physiological risk factors: Persistent or intense pain and discomfort during recovery are major contributors to postoperative depression. These are often exacerbated by reactions to anesthesia or pain medications, which can also cause fatigue, grogginess, and mood shifts. Recognizing these changes can help you identify the signs and seek appropriate support.
Peer-Reviewed Research: Mental Health Risk Factors
In the case of cosmetic and reconstructive surgery, there are many factors to take into consideration. Certain procedures, particularly major ones, may carry a higher risk of these emotional challenges. However, planning and surrounding yourself with a strong support system can help ease the healing process.
- Cosmetic, non-gender-affirming, plastic surgery: Research suggests that it doesn’t always lead to lasting improvements in mental health. If you have experienced depression, anxiety, or self-doubt in the past, you may find these feelings sticking around after surgery, and in some cases, they could even feel stronger. Research shows that satisfaction with physical changes after surgery doesn’t always translate to improved psychological well-being. If you’re considering a procedure, take the time to reflect on your motivations, discuss your expectations with your surgeon, and ensure you have a solid support network.
- Reconstructive surgery: Some patients experience temporary feelings of sadness or anxiety during recovery, sometimes related to financial stress, post-surgical pain, or adjusting to their new appearance. This is more often recorded in cases of spinal surgery, cardiac surgery, and others.
But remember, emotional preparation continues even after the procedure. The recovery process involves not only physical healing but also navigating emotional highs and lows.
Ultimately, a balanced and thoughtful approach fosters both physical and emotional well-being throughout the experience. Research shows that satisfaction with physical changes after surgery doesn’t always translate to improved psychological well-being. If you’re considering a procedure, take the time to reflect on your motivations, discuss your expectations with your surgeon, and ensure you have a solid support network. Prioritizing your emotional well-being alongside the physical changes will help you navigate the process with confidence and satisfaction.
Gender-Affirming Surgery
If you’re considering gender-affirming surgery, research consistently shows high satisfaction rates among individuals who have undergone these procedures. Please note that postoperative depression is common as a temporary, short-term experience; in the long term, patient satisfaction rates are astronomical for gender-affirming procedures.
- Studies indicate that most people feel positively about their surgical outcomes, with dissatisfaction being rare and typically linked to factors such as pre-existing psychological challenges or surgical complications..
- A review of thousands of cases reinforces these positive outcomes, showing regret after gender-affirming surgery is rare, affecting only about 1 percent of patients. Beyond overall satisfaction, different types of gender-affirming procedures—such as top surgery, facial feminization surgery, and bottom surgery—also show consistently high success rates. Studies indicate that these procedures, when performed with appropriate patient selection and care, lead to significant improvements in body image, reduced gender dysphoria, increased confidence, and enhanced overall well-being.
Remember, your decision is deeply personal, and embracing the process on your terms is essential. Taking the time to explore your options, seeking advice from experienced professionals, and ensuring your decision reflects what is right for you will help you achieve the best possible outcome.
Warning Signs and Symptoms of Post-Operative Depression
Postoperative depression is an important health concern that should never be overlooked. While gender-affirming surgery is typically associated with a sense of excitement for what lies ahead, it’s not uncommon for some patients to be very emotional while healing. It can be quite unsettling to grapple with post-surgery depression and anxiety. However, by recognizing the signs early on, you can take steps towards seeking the support you need.
If you notice persistent feelings of sadness, anxiety, or emotional distress after surgery, it’s important to talk about it with your support network, a mental health professional, and your surgical care team. Depression is not just a passing phase—it’s a medical condition that requires attention and care.
Common Emotional Symptoms of Postoperative Depression:
- Persistent sadness or low mood
- Loss of interest in activities once enjoyed
- Feelings of hopelessness or helplessness
- Increased irritability or frustration
- Difficulty concentrating or making decisions
- Changes in appetite or sleep patterns
- Fatigue or lack of energy
- Anxiety or excessive worry about recovery
- Feelings of guilt or worthlessness
- Thoughts of self-harm or suicide (seek immediate help)
If you or someone you know is struggling, reaching out for professional support can make a significant difference in healing.
Your support system
Undergoing any kind of surgery takes preparation, and it is important to have a strong support system in place. The person/people caring for you should be warm, encouraging, and not critical or afraid of your appearance or needs that come about during the healing process. You will need their full support during this time.
If you have a therapist…
Many people see a therapist on an ongoing basis. If you are currently seeing a therapist as part of your support system, then it is a very good idea to plan a session within 1-2 weeks of your surgery date, in case you experience symptoms of postoperative depression. Even though these feelings are temporary, it can be very helpful to talk about them. It is also important to let your therapist know you are having surgery before the day comes, so you can discuss coping mechanisms to put in place in case of potential postoperative depression, especially if you are already predisposed to depression.
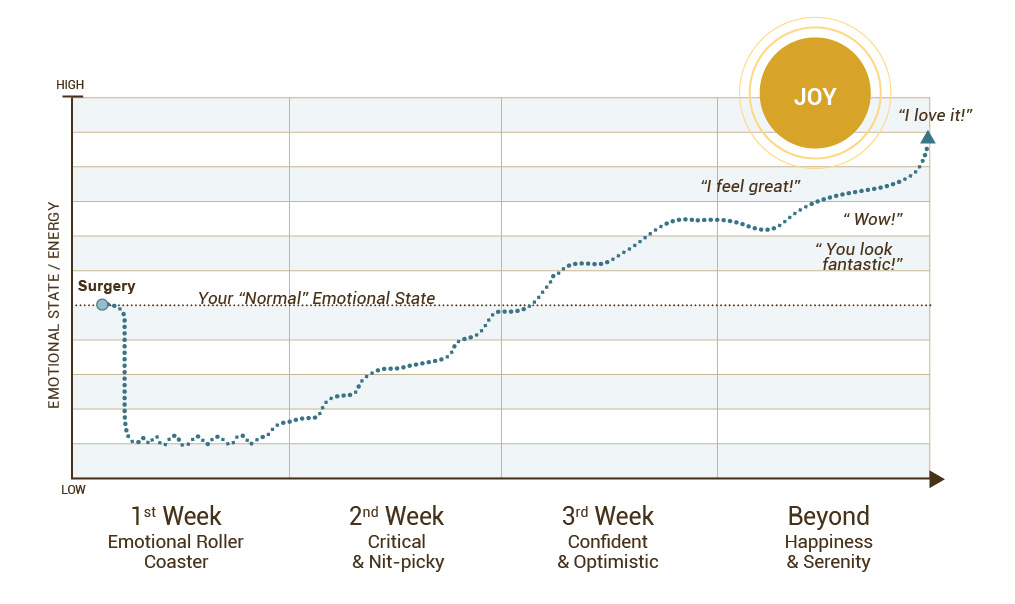
Below are some timelines to further explain what you may experience after surgery:
Emotional Roller Coaster
Please note that the following timeline is a rough estimation of the emotional experiences most patients have when recovering from top surgery. That said, every recovery process is unique. Not to mention, during the recovery process for many facial surgery and bottom surgery procedures, most patients experience longer spells of temporary, post-operative depression. This is due to greater amounts of pain, inflammation, and longer recovery times.Generally speaking, the emotional recovery period depends on the amount of procedures you undergo, your general health (both physical and mental) going into surgery, the type of support you receive, and other factors. The symptoms and timelines listed below may vary:
- The Day of Surgery: Tired, ‘out of it’, sleeping a lot
- 2–7 Days Post-Surgery: Exhaustion, anxiety, sadness, irritability, perhaps doubting the decision to have surgery
- 8–14 Days Post-Surgery: Hyper-critical, impatient, scared, eager for the recovery period to end and to get back to your regular life
- 15–21 Days Post-Surgery: Noticing results, feeling more positive, more confident in your decision to have surgery
- 1 Month Post-Surgery: Boost in confidence, happy you went through with it, getting positive reactions from others
- Beyond: Outcomes keep improving as healing continues
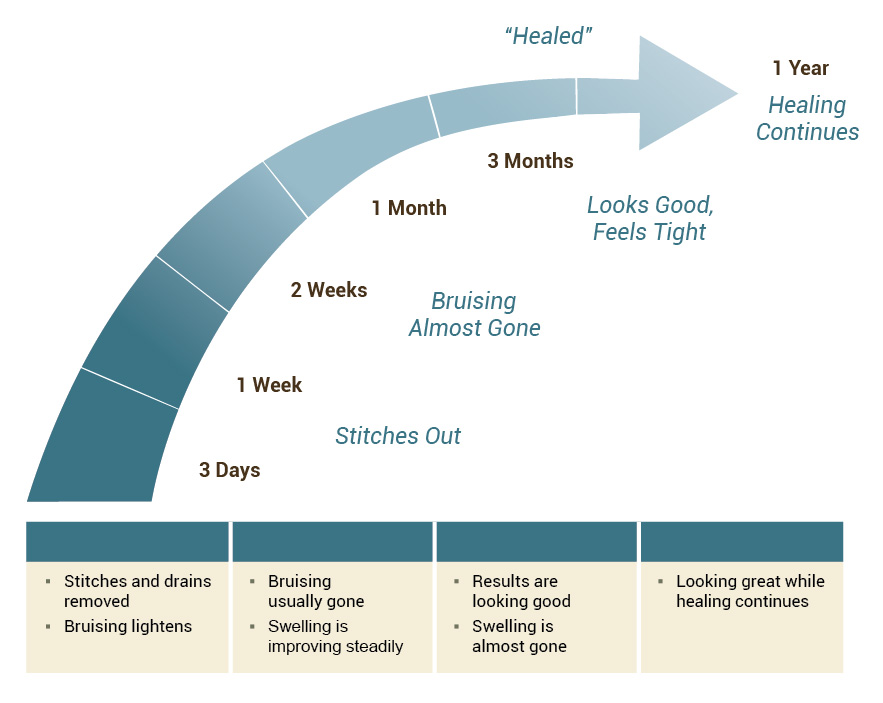
The Healing Curve
The diagram below was made to describe the healing timeline of patients who undergo chest reconstruction top surgery. Please note that it may not apply to all surgical healing recovery timelines.
Physical reactions: swelling
Many patients ask when the swelling will go away. This curve will help you understand that it is a gradual process. Swelling can last much longer than expected, but it will eventually go away.
Temporary versus Long-Term Post-Operative Depression
Emotional ups and downs are common after surgery, and most patients notice improvement as their body heals. Complications that cause ongoing pain, like fibrosis and chronic pain after top surgery due to inadequate scar care, or issues that extend recovery time, can also increase the risk of prolonged emotional distress. Research shows that unexpected surgical outcomes and longer-than-anticipated recovery periods can significantly affect mental health, making it especially important to set realistic expectations and maintain open communication with your surgical care team.
For many patients, post-surgical depression eases around the three-week mark, but recovery timelines vary depending on the procedure. More extensive surgeries, like bottom surgery or facial surgery involving multiple steps, may take longer, and complications, such as urethral issues after bottom surgery, can prolong the healing process. This can lead to extended periods of discomfort, reliance on others for support, and delays in resuming normal activities, which can affect emotional well-being.
If your mood hasn’t improved after two to three weeks or if your symptoms feel overwhelming, contact your surgical care team. They can help assess what’s going on and provide guidance to support your physical and emotional recovery.
Tips for Support and Coping with the Emotional Ups and Downs of Recovery
Planning for gender-affirming surgery is a deeply personal journey that involves practical and emotional preparation. From setting realistic expectations to ensuring a strong support system, taking thoughtful steps now can empower you to approach surgery with confidence and clarity. Here are key areas to consider as you prepare for surgery and recovery:
-
- Setting realistic expectations during your consultation: Understanding the potential results, recovery time, and limitations of the surgery helps ensure that your expectations align with what the procedure can realistically achieve.
- Budgeting and saving for surgery: Finances can be a major stressor after surgery. Saving up for recovery as well as surgery, preparing to take time off work, and familiarizing yourself with financing and grant opportunities can help.
- Organizing your recovery support: Recovery requires time and care. Arranging for help with meals, transportation, and daily tasks in advance can make the healing process more manageable. Having a clear recovery plan allows you to focus on healing without unnecessary stress.
- Emotional support: Recovery involves not only physical healing but also emotional development. We highly recommend that you take caution to surround yourself with compassionate, non-judgmental people while you recover. Likewise, if you have a therapist or counselor, plan to check in with them during recovery.
- Diet and exercise: Proper nutrition aids in recovery. Many patients find that spending time outdoors and engaging in light physical activities enhances their emotional and physical well-being.
Frequently Asked Questions About Post-Op Depression
Is it normal to get postoperative depression and anxiety?
Yes, temporary feelings of depression and anxiety after surgery are common and typically resolve as the body heals. Many patients experience emotional ups and downs during recovery, especially in the first few weeks when physical discomfort, limited mobility, and changes to routine can feel overwhelming.
Certain factors may increase the risk of post-surgical depression, including:
- Having a history of mental health conditions, such as anxiety or depression
- Facing complications that prolong recovery, such as chronic pain or mobility issues
- Dealing with external stressors like financial strain or lack of social support
If feelings of sadness or anxiety persist beyond the expected recovery period or if they begin interfering with daily life, it’s important to seek help from a mental health professional or your surgical care team.
How long does post-surgery depression last?
When it comes to recovery, there’s no one-size-fits-all answer. Each person heals at their own pace, and the complexity of the procedure plays a significant role in this process. For example:
- Transgender mastectomy patients: If post-op depression occurs, it typically starts to ease around week three.
- Breast cancer mastectomy patients: Depression may last longer due to the emotional weight of the procedure, as it can represent an unwanted loss, which can initiate a mourning process that some patients need to navigate as they work towards healing.
- Facial feminization surgery (FFS) and vaginoplasty: While FFS tends to have a more intense peak of pain, vaginoplasty recovery takes longer, impacting the return to normal activities like urination without a catheter or engaging in sexual activity. These challenges can extend the timeline for post-op depression.
Be kind to yourself and remember that, especially now, it’s important to give yourself proper time to heal. It’s perfectly normal to feel extra pressure and difficulty having to deal with all the trials of everyday life, with the added complication of less faculty, limited movement, isolation, vulnerability, and changes to routine.
How long does post-surgery anxiety last?
Recovery can bring about a range of emotions, and it’s important to recognize that anxiety may manifest differently for each individual, much like post-op depression. Factors that may contribute to anxiety during recovery include:
- Swelling: Patients may feel impatient while waiting for swelling to subside, as recovery times vary depending on the specific procedure.
- Healing complications: Delays in recovery caused by factors such as infections or mobility restrictions can lead to prolonged anxiety.
When should I seek help?
If you continue to experience significant depression or anxiety three weeks after surgery, please contact your surgical care team and a mental health professional.
Depression and anxiety can be considered complications of surgery, and monitoring your emotions is just as important as monitoring physical symptoms. Keeping a journal to track your feelings over time can help you identify patterns and pinpoint what contributes to emotional distress. If symptoms worsen instead of improving, professional support can help.
How can I support a friend who is experiencing postoperative depression and anxiety?
Supporting a patient during recovery can greatly enhance their experience and increase their chances of success. Your encouragement can be a significant catalyst for healing. Consider these approaches:
- Active listening, not judgment: Let them express their emotions without trying to “fix” the situation.
- Educate yourself: Learn about their type of surgery and common recovery experiences to better understand what they’re going through.
- Validate their feelings: Reassure them that their emotions—both positive and negative—are a normal part of the healing process.
- Celebrate their victories: It’s important to celebrate their victories, big and small. While recognizing progress is vital, acknowledging struggles is also a crucial part of the healing process, as it allows us to honor the milestones achieved.
- Help them connect with resources: Encourage them to explore online forums (like Transbucket and Transgender Map), support groups, and therapists who specialize in gender-affirming care. Connecting with others and accessing professional guidance can greatly impact their journey.
Click Here to Request the Next Steps to Schedule a Consult!
We offer complimentary virtual and in-person consultations with our board-certified surgeons. Click here to complete our consultation request form to learn more about the next steps in your patient journey.
BOOK CONSULTATION