Top Surgery Scars: Prevention, Healing, and Treatment
Medically reviewed by Paul Gonzales on February 27, 2024.
The visibility of scars is one of the most common concerns for patients who undergo top surgery–also called chest reconstruction, gender-affirming breast reduction, FTM top surgery, and non-binary top surgery. The most commonly asked questions pertain to the scars associated with double incision top surgery, although the periareolar and keyhole incisions are known to result in less visible scarring in certain cases. For those interested in reducing scar appearance, we begin with a list of preventative methods: the kinds of top surgery incisions that minimize scarring and pre-operative tips. Then, we go over healing protocols and treatment options for possible complications.
While some patients have concerns about visible scars, we acknowledge that not everyone shares this experience. Many patients proudly embrace their top surgery scars as a gift to themselves, symbolizing their journey towards alignment with their bodies and the experience of gender euphoria.
What will scars look like for different types of top surgery?
Chest reconstruction top surgery results in the appearance of scars that will vary in size and location based on the type of surgical techniques used. For example, less invasive procedures like keyhole and periareolar top surgery typically result in smaller, less noticeable scars near the areola (the pigmented area around the nipple). Conversely, more invasive methods like double incision top surgery generally result in more apparent scarring and will depend on how each person heals.
- Keyhole incisions – This technique is usually only successful on very small chests. Incisions are placed on the lower circumference of the areola.
- Periareolar incisions – Patients with small-to-medium-sized chests may benefit from this technique. Incisions extend completely around the border of the areola.
- Double incisions – Large chests require a larger incision to address excess skin and tissue. This technique involves a horizontal or curved incision(s) on the skin just beneath the chest muscle border. Another incision is also made around the areolas to relocate the nipple.
How long does it take for top surgery scars to heal?
Incisions can take up to 12 months to fully heal and develop into mature scars. For this reason, we recommend that you keep your scars out of the sun or at the very least protected with sunscreen for your first year after surgery. Upon request, your surgeon can provide you with other personalized recommendations about what you can do to advance the healing of your scars post-op in a free, virtual consultation. We elaborate more on these care and prevention methods below.
What factors contribute to abnormal scarring?
Scars vary in appearance among individuals and are influenced by how each person heals. While there are many precautionary steps a patient can take to reduce the size and discoloration of their scars, some patients might have genetic predispositions that make them more likely to develop visible scars. We discuss all of these factors below:
- Skin tone – Normally, scars appear slightly lighter than the surrounding skin but may be more visibly apparent in people of color, especially those with more pigmented skin.
- Genetic predisposition – Some are more predisposed to abnormal scarring, which can manifest in scars appearing much lighter in color than surrounding skin (hypopigmented scars), or scars that are raised or thickened (hypertrophic scars) that may extend beyond the original boundaries of the incisions (keloids). Keloid formation may be more common in individuals with a family history.
- Wound healing process – Infections or other factors that increase or prolong inflammation around the incisions during the wound healing process can manifest in any form of abnormal scarring.
- Raising arms and stretching forces – While evidence suggests stretching forces may worsen abnormal scar formation, there’s ongoing debate among healthcare providers about restricting arm mobility after top surgery, particularly with raising the arms above the shoulder, within the first 6 months after top surgery until scars are fully healed. Balancing the risk of widening scars with preserving long-term shoulder mobility is crucial, especially for patients prone to joint issues or with existing joint conditions.
- In collaboration with physical therapy experts, our surgeons recommend patients at GCC to limit arm movements below shoulder level within the first 3-4 weeks after top surgery to reduce stretching forces on the incisions.
- We recommend patients consult with a physical therapist to progressively increase their mobility 4 weeks after top surgery. We’ve created a free physical therapy rehabilitation guide detailing a timeline of recommended post-op exercises to enhance their recovery process.
- Other factors – High blood pressure, depending on clinical severity, may lead to the formation of keloids and hypertrophic scars, due to its damaging effects on blood vessels, resulting in increased inflammation. Other factors like young age (common in 20s-30s) and pregnancy may also impact the development of keloids suggesting hormonal factors may play a role.1
What can I do before surgery to minimize the appearance of my scars?
While scars are unavoidable after top surgery, having good overall health helps to support a proper wound healing process to minimize abnormal scar formation.
- Maintaining overall health – Certain health conditions or medications can impact your body’s wound healing process. For example, individuals with autoimmune conditions requiring immunosuppressants may experience delayed wound healing, which may affect scar formation. Regardless of your overall health, consulting with a primary care physician is advisable to ensure you’re fit to undergo surgery.
- Avoid smoking or nicotine use – If applicable to you, avoid smoking or using nicotine for at least 3 weeks before AND after surgery as they can impair blood flow to tissues, resulting in poor wound healing.
- Proper nutrition and supplements – Eating a nutritious diet that contains adequate protein, zinc, and vitamin C, all of which have been clinically proven to accelerate wound healing, is key to help prepare you for recovery and healing before surgery.
What does scar management look like after surgery?
Below is a relative timeline and general outline of different forms of scar management after top surgery. You can learn more about how to care for your scars here and how to minimize them with this downloadable PDF about scar management.
- Compression and incision care – Recommended within the first 3 weeks after surgery for proper wound healing. Compression binders/garments help minimize swelling while incision care through dressing changes and/or antibacterial ointments help reduce the risk of infections.
- Silicone-based scar treatments and scar massage – Recommended 3 weeks after surgery to regulate the scar formation process. Silicone tape or gel creates a protective barrier, keeping the scar moisturized and soft. Additionally, scar massage aids in flattening and smoothing out the developing scar tissue.
- Reducing sun exposure – Advised within the first 6 months after surgery to minimize hyperpigmentation of scars. Protection with sunscreen or clothing over the scars is recommended.
What non-surgical treatments exist for abnormal scarring?
If additional scar management is required, various treatments involving needles or lasers can enhance the appearance of scars.
- The following procedures are typically performed with clearance from your surgeon starting 3 months after surgery. Treatments may require at least 2-3 sessions (or more) every 4-6 weeks before results are noticeable.
- Steroid injections reduce inflammation and break down excess collagen that may lead to widened or thickened scars. GCC patients can receive the first 3 complimentary injections in-office.
- Microneedling/Micropen uses fine needles to create controlled micro-injuries in the scar, stimulating new collagen production, and triggering wound healing process to improve the appearance or texture of scars.
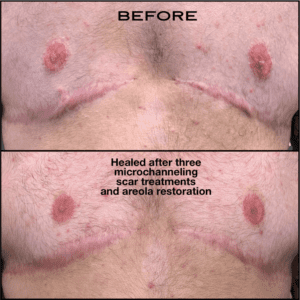
- Microchanneling uses a special device to create channels that allow for the delivery of stem-cell serums or other skin care products to deeper layers of the skin to increase their efficacy. May be started as early as 6-8 weeks with surgeon clearance. Below is a before and after photo set of a top surgery patient done by Jen Lee in San Francisco.
-
- Broad band light (BBL) is a form of light therapy used to reduce redness or hyperpigmentation that may be seen in some scars.
-
- Laser therapy may also be used to reduce redness and thickness of scars.
- Medical tattooing – Generally performed 12 months after surgery to allow the scar to fully mature and allow pigment to settle. A qualified medical tattoo artist employs their expertise in color theory to match the scar with the natural skin tone to effectively camouflage it. Below you can find a before and after picture of scar camouflage tattooing done by Candace Falcon of Falcon Artistry Tatoo. Patients who wish to cover their scars with decorative tattoos should also wait 12 months post-op before doing so.
What is a scar revision surgery? Why might someone want it?
A scar revision surgery involves excising the original scar to create a new one. Patients tend to opt for revision surgery to treat their scars if complications are a result of tension created during the initial recovery process. Scars created during a revision surgery tend to heal nicer. In other words, they end up being less visually apparent because less tension is put on the incision than in the initial surgery when the chest was reconstructed.
A scar revision surgery can be performed 6-12 months after your initial top surgery to ensure the scar formed is mature and won’t change before it is surgically removed. This will allow the surgeon to create a new and less noticeable scar.
Identifying & Treating Keloid & Hypertrophic Scars
In this informational video, Dr. Alexander Facque (he/him) explains the difference between keloid and hypertrophic scars as well as how they can be treated.
Conclusion
- Scars vary based on surgery type, with keyhole and periareolar surgeries resulting in smaller scars and double incision surgery leading to more apparent scarring.
- Skin tone, genetics, wound healing process, and stretching forces affect scar appearance.
- Maintaining overall health, avoiding smoking, and proper nutrition support optimal wound healing.
- Proper wound care, silicone-based treatments, scar massage, sun protection, non-surgical treatments, and medical tattooing can improve scar appearance. Scar revision surgery is an option to surgically remove old scars, creating a newer, less noticeable scar. When it comes to aftercare, each surgeon will give you their own recommendations based on their experience and preferences. Dr. Jacobs (he/him), for example, recommends compression over all other care techniques. Still, patients should follow other care protocols like being careful not to expose their scars to UV rays during the first year after recovery.
Sources
Request a Free Surgical Consultation Today.
All virtual and in-person consultations with our board-certified surgeons are free. Once you fill out this form, our patient care team will reach out and guide you through every step to get to surgery.